Pain and the Pelvic floor
Written by Lindsey Tasker Cole, MPT, BSc.Kin | May 18, 2021
When you google pelvic pain the list is long, like really long! This makes sense because yes, there are many reasons one might experience pelvic pain! And sometimes there are multiple reasons combined that can result in chronic pelvic pain. SO, let’s dive into it!
Pelvic pain can arise from your digestive, reproductive or urinary system, and/or your musculoskeletal system. Recently doctors have recognized that some pelvic pain, particularly chronic pelvic pain, can also arise form muscles and the connective tissue in the structure of the pelvic floor (1). Occasionally, and more often than not, pelvic pain might also be caused by irritation or sensitivity of the nerves in the pelvic girdle. Pelvic pain may be acute, recurrent or chronic. It is generally agreed if someone has pain for more than 3- or 6-months duration and is located primarily in the pelvic – it is considered chronic. (2)
The anatomical integrity and proper functioning of the pelvic floor muscles and their associated neural, vascular, and connective tissue structure, as well as the interplay between them are essential for some of the primary functions of life. This includes the stability of the lumbar spine, pelvis and hips, support of the pelvic organs (bladder, uterus, ovaries, rectum); storage and evacuation of urine and feces; and sexual function. Impairment and/or pain affecting the pelvic floor muscles directly or indirectly (via related organs) may result in dysregulation of any of these body systems and functions (3).
Pelvic floor muscle dysfunction is often thought of in terms of hypotonic, damaged and/or weakened muscles, associated with disorders such as urinary and fecal incontinence and pelvic organ prolapse. Several other conditions, such as elimination disorders of the bladder and bowel, sexual dysfunction, and genital/pelvic pain syndromes are also commonly associated with pelvic floor muscles dysfunction. But in these cases, the muscles are thought to be hyperactive (overactive) and consequently hypertonic. We refer to this state of the pelvic floor as the ‘overactive pelvic floor’ (OAPF) (3).
Symptoms and conditions associated with OAPF are common and may significantly affect the health of women, men and children. If this condition is the primary problem or secondary in response to something else, it is considered to be a significant cause of pelvic floor dysfunction and more importantly pain (3).
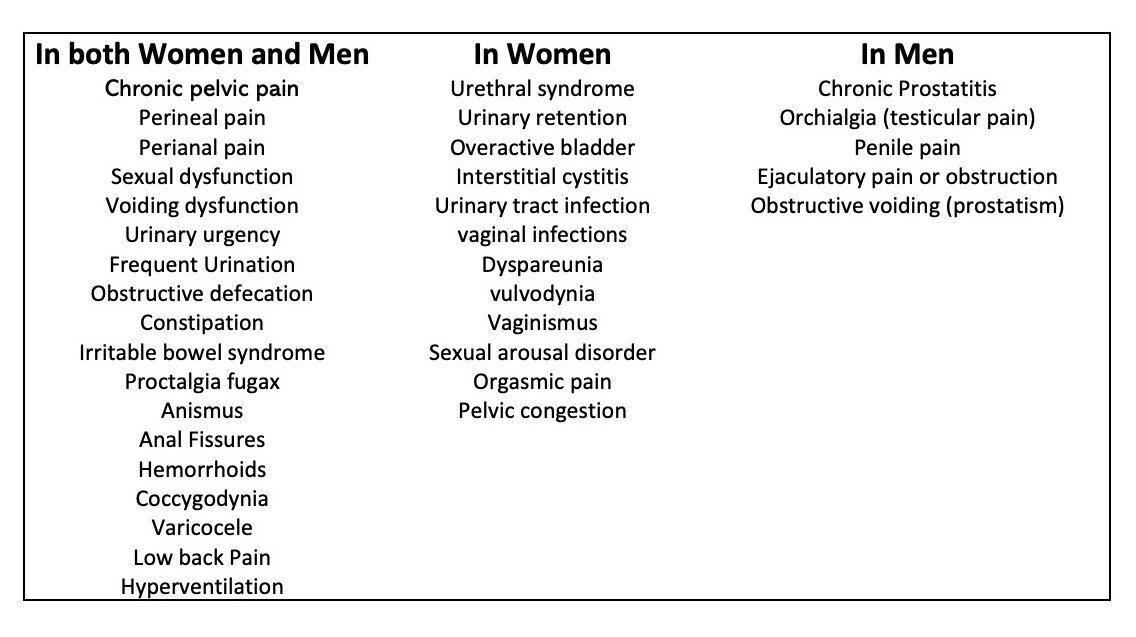
This condition of the pelvic floor is often missed, and this is why it is so important to have a very thorough and history and physical exam to ensure the right course of treatment is implemented. Some of the symptoms of OAPF are put together in a chart below: (4,5,6,7,8)
If you are experiencing any of the symptoms listed above or have questions, just know there is help available. Some of these issues are very sensitive and can be difficult to bring up but can also be significantly affecting your quality of life. There is treatment and help available, and the team at Holistic will be more than happy to get to you started in the right direction. Follow up with your health care team to make sure you are not just surviving, but you are thriving!
Lindsey Tasker Cole
Psysiotherapist, Pelvic Health Therapist, Vestibular Physiotherapist
Resources:
1. Mayo Clinic - https://www.mayoclinic.org/symptoms/pelvic-pain/basics/causes/sym-20050898
2. El-Minawi, A. M., Perry, C. P., Carter, J. (2000). Pelvic Pain: Diagnosis and Management. United Kingdom: Lippincott Williams & Wilkins.
3. The Overactive Pelvic Floor. (2015). Germany: Springer International Publishing.
4. Van Lunsen RHW, Ramakers MJ. The hyperactive pelvic floor syndrome (HPFS): Psychosomatic and psycho-sexual aspects of hyperactive pelvic floor disorders with co-morbidity of uro-gynaecological, gastro-intestinal and sexual symptomatology. Acta Endosc. 2002;32(3): 275-85
5. Butrick CW. Pathophysiology of pelvic floor hypertonic disorders. Obstet Gynecol Clin North Am. 2009; 36 3): 699-705
6. Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstet Gynecol Clin North Am. 2009 ;36 (3) 707-22
7. Fitzgerald MP, Kotarions R. Rehabilitation of the short pelvic floor I: background and patient evaluation. Int Urogynecol J pelvic Floor Dysfunct. 2003; 14 (4): 261-8
8. Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Maya Clin Proc. 2012; 87 (2): 187-93